Introduction
As approaches to pain management evolve, healthcare professionals rely heavily on evidence-based guidelines to determine the safest and most appropriate treatment paths for different types of pain. Within these frameworks, medications containing tapentadol—such as Aspadol 150 mg—are often referenced in discussions about chronic or severe pain where both nociceptive and neuropathic elements are present. While these medications play a role in certain clinical settings, current guidelines emphasize careful evaluation, risk assessment, and structured monitoring when considering any opioid-like agent.
This comprehensive guide explores where Aspadol 150 mg fits within today’s pain management recommendations, how its pharmacological properties contribute to its clinical relevance, what research indicates about its use, and what safety principles guide responsible prescribing.
1. Understanding Aspadol 150 mg: Pharmacological Foundations
To understand Aspadol 150 mg’s place in pain management guidelines, it is essential to first examine the medication’s pharmacological characteristics. Aspadol contains tapentadol, a centrally acting analgesic known for its dual mechanism of action, which makes it distinct from traditional opioids.
1.1 Dual Mechanism of Action
Tapentadol functions through:
-
Mu-opioid receptor (MOR) activation
-
Supports the modulation of pain signals in the central nervous system
-
Targets nociceptive pain components
-
Offers analgesic effects similar to traditional opioids, though with a different receptor affinity profile
-
-
Norepinephrine reuptake inhibition (NRI)
-
Enhances descending inhibitory pain pathways
-
Useful for neuropathic or mixed pain types
-
Often cited as an advantage for chronic musculoskeletal and nerve-related pain
-
1.2 Why Mechanism Matters in Guidelines
Pain guidelines tend to categorize medications by mechanisms and risk profiles. Because tapentadol interacts with opioid receptors and influences neurotransmitter activity, it is placed among centrally acting analgesics requiring cautious, structured use.
Its dual mechanism also positions it as a candidate in treatment-resistant pain cases—but only after non-opioid and non-pharmacologic strategies have been evaluated.
2. Overview of Current Pain Management Guidelines
Pain management guidelines increasingly focus on balancing relief with safety, especially due to global concerns surrounding opioid risks. Most guidelines—whether from pain societies, national health organizations, or medical boards—share several common themes.
2.1 Emphasis on Non-Opioid and Non-Pharmacologic Care First
Before considering medications like Aspadol 150 mg, clinicians are generally encouraged to prioritize:
-
Physical therapy
-
Cognitive-behavioral interventions
-
Lifestyle modifications
-
Non-opioid analgesics (acetaminophen, NSAIDs when appropriate)
-
Neuropathic agents (anticonvulsants, antidepressants)
These strategies form the foundation of modern multimodal pain management.
2.2 When Centrally Acting Analgesics Are Considered
Guidelines typically reserve opioid-like medications for:
-
Chronic pain not responding to first-line measures
-
Pain with confirmed functional impairment
-
Cases where benefits may outweigh potential harms
-
Conditions involving mixed neuropathic and nociceptive elements
-
Treatment plans that include regular follow-up and reassessment
2.3 Ongoing Reassessment Requirements
Most guidelines emphasize:
-
Periodic monitoring of pain levels
-
Assessment of functional improvement
-
Surveillance for side effects
-
Evaluation for signs of misuse
-
Dose adjustments or discontinuation if benefits decrease
These principles directly shape how a medication like Aspadol 150 mg is used in clinical settings.
3. Aspadol 150 mg’s Place in Guideline-Based Pain Management
Although guidelines vary by region, several shared principles clarify where Aspadol 150 mg may fit—always under clinical supervision.
3.1 Potential Role in Chronic Musculoskeletal Pain
Tapentadol-containing formulations are sometimes discussed in guidelines for chronic musculoskeletal pain, including:
-
Low-back pain
-
Osteoarthritis with neuropathic features
-
Post-traumatic pain syndromes
However, its use typically follows failure or insufficient response to:
-
Non-opioid therapies
-
Physical interventions
-
Behavioral strategies
-
Adjuvant analgesics
This aligns with the stepwise approach emphasized in almost all clinical frameworks.
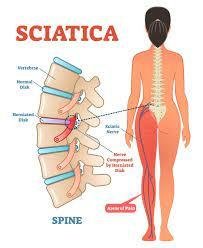
3.2 Role in Neuropathic and Mixed Pain
Tapentadol’s norepinephrine reuptake inhibition mechanism has drawn interest for neuropathic pain conditions. Guidelines acknowledge its potential role after first-line neuropathic agents—such as gabapentinoids or serotonin-norepinephrine reuptake inhibitors—are explored.
Examples of chronic neuropathic pain where tapentadol is sometimes discussed include:
-
Diabetic neuropathy
-
Radicular pain
-
Neuropathic components of musculoskeletal disorders
Again, guidelines emphasize careful patient selection and ongoing monitoring.
3.3 Consideration in Moderate-to-Severe Pain Situations
For carefully selected patients who experience significant pain despite optimized non-opioid strategies, centrally acting analgesics like Aspadol 150 mg may be introduced within the context of:
-
A documented treatment plan
-
Clear therapeutic goals
-
Evaluation of risk factors (including substance use history)
-
Regular follow-up evaluations
This approach supports both effectiveness and safety.
4. What Recent Research Reveals About Tapentadol-Based Medications
Recent studies have contributed to a more nuanced understanding of tapentadol’s role in chronic pain.
4.1 Improved Functional Outcomes in Certain Populations
Some studies indicate that tapentadol may help improve:
-
Mobility
-
Sleep
-
Daily physical functioning
-
Overall quality of life markers
These outcomes are significant because modern guidelines emphasize functional improvement—not just pain reduction—as a primary treatment objective.
4.2 Potential Benefits for Mixed Pain Syndromes
Individuals with mixed pain often present challenges in treatment. Research suggests tapentadol’s dual mechanism may offer advantages where single-mechanism analgesics fall short.
4.3 Reduced Polypharmacy in Some Cases
In certain studies, patients using tapentadol required fewer additional analgesics, which may reduce risks associated with medication combinations.
However, all such findings are balanced by guideline emphasis on risk awareness and ongoing evaluation.
5. Guideline-Based Safety Considerations for Aspadol 150 mg
Because Aspadol 150 mg involves opioid receptor activity, guidelines universally highlight the need for strict safety measures.
5.1 Monitoring for Side Effects
Common concerns may include:
-
Drowsiness
-
Dizziness
-
Respiratory risks
-
Gastrointestinal effects
-
Potential medication interactions
Careful monitoring ensures risks are identified early.
5.2 Avoiding Abrupt Dose Changes
Guidelines advise against sudden dose increases or discontinuations, as these can lead to complications.
5.3 Patient Education and Treatment Agreements
Clinicians are encouraged to:
-
Discuss risks
-
Outline expectations
-
Establish treatment goals
-
Use written agreements when appropriate
These measures improve safety and transparency.
5.4 Evaluating Risk Factors for Misuse or Dependence
Risk assessment tools are often used before initiating medications like Aspadol 150 mg.
These may evaluate:
-
Personal or family history of substance use
-
Mental health conditions
-
Polypharmacy concerns
-
Environmental and psychological factors
Guidelines emphasize tailoring decisions to each patient’s risk profile.
6. Aspadol 150 mg in Multimodal Pain Management Models
Multimodal pain care combines multiple methods to improve overall outcomes. In this approach, Aspadol 150 mg may be one component—never the sole treatment.
6.1 Common Components of Multimodal Care
-
Physical rehabilitation
-
Anti-inflammatory medications
-
Neuropathic agents
-
Psychosocial therapies
-
Occupational therapy
-
Lifestyle modification programs
Guidelines increasingly encourage this integrative model, which reduces reliance on any single medication.
6.2 Enhancing Outcomes Through Combination Approaches
Studies show better outcomes when centrally acting medications are paired with:
-
Movement-based therapies
-
Mindfulness methods
-
Educational programs
-
Strengthening/conditioning routines
This underscores guideline emphasis on holistic treatment rather than medication-focused care.
7. Future Directions for Aspadol 150 mg in Clinical Guidelines
As new research continues, guidelines may evolve. Current areas of interest include:
-
Long-term outcomes and safety
-
Effects on cognitive and physical function
-
Comparative effectiveness vs. other analgesics
-
Roles in emerging pain categories
-
Strategies for minimizing risks while optimizing relief
These ongoing investigations will shape Aspadol 150 mg’s place in future pain frameworks.
Conclusion
Aspadol 150 mg, containing tapentadol, holds a defined but carefully controlled place in modern pain management. While research indicates potential benefits—particularly for chronic, mixed, or neuropathic pain—current guidelines emphasize a cautious, structured, and individualized approach. Non-pharmacologic and non-opioid options remain the foundation of pain care, with medications like Aspadol 150 mg reserved for scenarios where other strategies have proven inadequate or insufficient.
Understanding how Aspadol fits into evidence-based clinical guidelines allows patients and clinicians to engage in informed, collaborative decision-making that prioritizes both safety and quality of life.
Frequently Asked Questions (FAQs)
1. Where does Aspadol 150 mg fit in pain management guidelines?
It is typically considered only after first-line therapies fail and when potential benefits outweigh the risks.
2. Why is Aspadol 150 mg discussed for neuropathic pain?
Tapentadol’s dual mechanism—including norepinephrine reuptake inhibition—makes it relevant for certain neuropathic or mixed pain conditions.
3. Is Aspadol 150 mg a first-choice therapy?
No. Guidelines recommend non-opioid and non-pharmacologic interventions before centrally acting analgesics.
4. What monitoring is recommended when medications like Aspadol are used?
Healthcare professionals monitor functional improvement, side effects, and any signs of misuse while reassessing treatment goals.
5. Does Aspadol 150 mg work alone or as part of a multimodal plan?
It is usually one component of a broader, multimodal pain management strategy.
6. Are guidelines likely to change as more research emerges?
Yes. Ongoing studies continue to refine understanding of tapentadol’s long-term safety and effectiveness.